Abstract
Carbon nanoparticles have recently drawn intense attention in biomedical applications. Hence, there is a need for further in vivo investigations of their biocompatibility and biodistribution via various exposure routes. We hypothesized that intraperitoneally injected diamond, graphite, and graphene oxide nanoparticles may have different biodistribution and exert different effects on the intact organism. Forty Wistar rats were divided into four groups: the control and treated with nanoparticles by intraperitoneal injection (4 mg of nanoparticles/kg body weight) eight times during the 4-week period. Blood was collected for evaluation of blood morphology and biochemistry parameters. Photographs of the general appearance of each rat’s interior were taken immediately after sacrifice. The organs were excised and their macroscopic structure was visualized using a stereomicroscope. The nanoparticles were retained in the body, mostly as agglomerates. The largest agglomerates (up to 10 mm in diameter) were seen in the proximity of the injection place in the stomach serous membrane, between the connective tissues of the abdominal skin, muscles, and peritoneum. Numerous smaller, spherical-shaped aggregates (diameter around 2 mm) were lodged among the mesentery. Moreover, in the connective and lipid tissue in the proximity of the liver and spleen serosa, small aggregates of graphite and graphene oxide nanoparticles were observed. However, all tested nanoparticles did not affect health and growth of rats. The nanoparticles had no toxic effects on blood parameters and growth of rats, suggesting their potential applicability as remedies or in drug delivery systems.
Similar content being viewed by others
Background
Carbon nanoparticles (CNP) are a promising type of biomaterial for diagnostic and therapeutic applications due to their high biocompatibility and low toxicity [1, 2]. Diamond nanoparticles (DN), graphite nanoparticles (GN), and graphene oxide (GO) are receiving increasing attention in biomedical sciences for a large variety of applications, including protein immobilization, biosensors, therapeutic molecule delivery, and bioimaging.
Among the chosen nanoparticles, DN have attracted the greatest attention in in vivo experiments due to their physicochemical properties such as chemical stability, small size, large surface area, high adsorption capacity, good biocompatibility [3, 4], and easy surface functionalization for photostable fluorescent and luminescent imaging [4–7]. It has been suggested that DN may prove to be an even better drug carrier [8], imaging probe [9, 10], or implant coating [11] in biological systems compared with other carbon nanomaterials. Moreover, in vivo studies have not observed any negative effects in laboratory animals. DN administered to mice over 6 months had no harmful effects on growth, fertility, immunity, and biochemical and morphological parameters of the blood [12–14].
In vivo toxicity of GN has not been extensively investigated yet. It has been reported that graphite nanoplatelets had no genotoxic or in vivo toxic effects on Caenorhabditis elegans [15].
Recently, the potential toxicity of graphene in biological systems has become of great concern [16–18]. It has been demonstrated that, after intravenous injection into mice, GO accumulated in the lungs, resulting in pulmonary edema and granuloma formation [17, 18]. Intravitreal injection of GO into rabbits’ eyes affected the eyeballs’ appearance, intraocular pressure, electroretinogram, and histological parameters [19]. On the other hand, surface-functionalized graphene or GO with improved water dispersity and better stability in physiological environments appear to be much less toxic [17]. Their intrinsic physical properties such as the strong light absorption and fluorescence of functionalized GO and its nanocomposites have been utilized for photothermal therapy of cancer and as a contrast agent for in vitro and in vivo imaging [20, 21].
CNP have a high potential to be used as a drug carrier; hence, there is a need to investigate various exposure routes and confirm that a chosen platform has no toxic impact on animal models. Local administration, like the intraperitoneal route of CNP, is sparsely investigated, but seems to be safe, convenient, rapid, and causing less animal stress than intravenous administration. We hypothesized that after injection, CNP may have different biodistribution and exert different effects on the intact organism. The objective of the present study was to evaluate the biodistribution of nanoparticles in the rat model with particular emphasis on the gross pathology, vascular system, and general animal condition after multiple injections of a high dose of CNP. Presented results are the first step describing in vivo biodistribution of CNP; the next steps will include micro- and ultrastructure examination, as well as evaluations at a molecular level.
Methods
Nanoparticles
Nanoparticle Suspensions
DN and GN were obtained from Skyspring Nanomaterials (Houston, TX, USA). Both nanomaterials were produced by the explosion method and synthesized to 3–4 nm. According to the manufacturer, the purity of DN was >95 % and it had a specific surface area of ~282 m2/g, while the purity of GN was >93 % and it had a specific surface area of 540–650 m2/g. GO were prepared from graphite nanoparticles by a modified Hummers method using natural graphite flakes (purchased from Asbury Carbons, Asbury, USA) in the Institute of Electronic Materials Technology (Warsaw, Poland) [22]. In a synthesis, 5 g of graphite was added into 600 mL of H2SO4 and 67 mL of H3PO4 acid mixture. KMnO4 (30 g) was added in portions. The reaction was kept at 50 °C with continuous stirring for 4 h. To stop the reaction, the mixture was poured on 5 mL of deionized water, and 10 mL of H2O2 was added. Oxidized graphite was purified by sedimentation and centrifugation until concentrated suspension had pH 7. In the next step, the suspension was diluted with deionized water to 250 mL and was subjected to sonication by 500 W ultrasound processor with 75 % amplitude for 5 min. Dry powder was obtained via freeze-drying process. The diameters of the GO particles ranged from 8 to 25 nm. The physical characteristics of the nanoparticles are given in Table 1.
The nanoparticle powders were suspended in sterile saline solution to a concentration of 500 mg/L and sonicated at 550 W/m2 for 1 h in an ultrasonic bath (Sonorex Super RK 514H, Bandelin Electronic, Germany) before each injection.
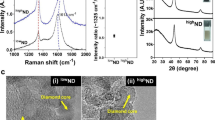
Visualization of Nanoparticles
The size and shape of nanoparticles were inspected using transmission electron microscopy (TEM: JEM-2000EX; JEOL, Tokyo, Japan) at 80 keV. Images were captured with a Morada 11 megapixel camera (Olympus Soft Imaging Solutions GmbH, Münster, Germany). Droplets of sample solutions were placed onto Formvar-coated copper grids (Agar Scientific, Stansted, UK), and immediately after air-drying, the grids were inserted into the TEM (Fig. 1a–c). The macroscopic structure of the nanoparticle powders was visualized using a Nikon D7000 digital camera with a Nikon AF-S Micro-Nikkor 105mm f/2.8G IF-ED VR lens (Nikon, Tokyo, Japan) (Fig. 1d–f).
The DN (Fig. 1a) and GN (b) had a spherical shape. The DN powder was cinnamon brown (d), while the GN powder was the darkest and mostly fine-grained (e). The shape of GO was an irregular single layer (c), and the powder was dark brown (f).
Zeta Potential Measurements
The Zeta potential and size distribution of suspended nanoparticles were determined after 120 s of stabilization at 25 °C by the dynamic laser scattering-electrophoretic method with Smoluchowski approximation by Zetasizer Nano-ZS90 (Malvern, Worcestershire, UK). Each measurement was repeated three times. The mean Zeta potentials of the DN, GN, and GO solutions in 0.9 % NaCl were −15.8, 12.5, and −8.80 mV, respectively (Table 1).
Animals
Animal Maintenance
The experiments were performed in accordance with Polish legal regulations concerning experiments on animals (Dz. U. 05.33.289). The experimental protocols were approved by the local ethics commission for experimentation on animals.
Forty female Wistar/cmdb outbred rats (6 weeks old, 124 ± 12 g body weight (BW)) were randomly divided into four groups (control, DN, GN, GO) and kept in polycarbonate cages with steel wire tops. They were kept under standard conditions at a room temperature of 22 ± 2 °C, 50–60 % humidity, and 12:12 light-dark cycle (lights on at 7 a.m.).
The animals had free access to water and dry pellet feed (Labofeed B standard, Wytwórnia Pasz ‘Morawski’, Poland). During the whole experiment, animal behavior and hair/skin condition were monitored.
Administration of Nanoparticles
Rats received multiple intraperitoneal injections of 1 mL of physiological saline (0.9 % NaCl) for the control (placebo) group and 1 mL of nanoparticle suspensions in physiological saline for the treatment groups. The injections were given for 4 weeks at 3-day intervals (eight injections in total). The nanoparticle suspensions were given at a concentration of 500 mg/L, equivalent to 4 mg of nanoparticles/kg BW.
Animal Euthanasia
After 4 weeks of CNP injection, the rats were fasted overnight prior to blood collection. The animals were euthanized by inhalation of isoflurane (Forane, USP, Baxter Poland). The anesthetized animals were laid in dorsal recumbency during the cardiac puncture procedure, which was used to collect blood samples from the heart. Blood was collected for evaluation of blood morphology and biochemistry parameters. Photographs of the general appearance of each rat’s interior were taken immediately after sacrifice.
Weight Changes and Organ Indices
Individual rats were weighed at the beginning of experiment, prior to every injection and shortly before euthanasia. The mean BW of the groups was plotted against time to reveal the course of BW gain. The rats were sacrificed and their organs were excised and weighed. The macroscopic structure of the organs was visualized using a stereomicroscope (Olympus, SZX 10, Tokyo, Japan).
Biochemical Serum Parameters and Hematology Measurements
Blood was collected in 5 mL tubes with a coagulation activator and 1 mL tubes with K3-EDTA. All biochemical parameters were assessed using a Miura One Clinical Chemistry Analyzer (I.S.E., Guidonia, Italy), and the reagents were purchased from Pointe Scientific Inc. (Canton, USA). Blood collected in the tubes with a coagulation activator was centrifuged at 3800 × g for 8 min at 4 °C for hemolysis-free serum collection. The biochemistry of the hemolysis-free serum was analyzed by standard laboratory procedures. The following parameters were examined: aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), glucose, creatinine, blood urea nitrogen (BUN), total protein (TP), albumin, lactate dehydrogenase (LDH), and triglycerides (TG).
Blood collected in the tubes with K3-EDTA was used for hematology examination, performed with an Abacus Junior Vet Hematologic Analyzer (Diatron Group, Budapest, Hungary). The following parameters of the whole blood were examined: number of red blood cells (1012/L), plasma hemoglobin concentration (g/dL), hematocrit (%), number of platelets (109/L), relative distribution width of the red cell population (% of covariance), red cell mean corpuscular volume (fL), mean erythrocyte hemoglobin concentration (pg), and mean cell hemoglobin concentration (g/dL). White blood cell subpopulations were quantified and expressed in absolute numbers (109/L): white blood cells, lymphocyte counts, granulocyte counts, and mid cell counts. The mean platelet volume (fL) and plateletcrit/relative volume of thrombocytes (%) were also determined.
Data Analysis
Statistical significance was determined by one-way analysis of variance (ANOVA) and Tukey’s test using Statgraphics® Plus 4.1 (StatPoint Technologies, Warrenton, VA, USA). Differences at P ≤ 0.05 were defined as statistically significant. All data are presented as mean ± standard deviation.
Results
Animals’ Body Condition/General Health Status
During the 4 weeks of injections, none of the animals showed physical or behavioral changes. Daily intake of feed and water and BW gain did not differ significantly between the groups (Figs. 2 and 3).
Macroscopic Evaluation of Organs
During macroscopic evaluation of the organs, no pathological changes were observed (Figs. 4f–j, 5f–j, 6f–j, and 7d–h). There were no significant differences in the mean organ weights between any of the groups (Table 2).
Visualization by digital camera of the biodistribution of diamond nanoparticles after multiple intraperitoneal injections into rats. Solid aggregates were lodged in injected body regions (a, b, c), small dots of nanoparticle aggregates were also present in abdominal lipid tissue (e) and mesentery (d). Black arrows indicate diamond nanoparticle aggregates. The macroscopic structure of the kidney (f), lungs (g), heart (h), spleen (i), and liver (j) were also examined. There were no macroscopic pathological features on the organs
Visualization of the biodistribution of graphite nanoparticles after multiple intraperitoneal injections to rats by digital camera. Solid aggregates were placed in injection body regions (a, b, c, e) and in mesentery (d), small dots of nanoparticle aggregates were in lipid tissue proximity spleen serosa (i). Black arrows indicate graphite nanoparticles aggregates. The macroscopic structure of the kidney (f), lungs (g), heart (h), spleen (i), and liver (j) were also examined. There were no macroscopic pathological features on the organs
Visualization of the biodistribution of graphene oxide nanoparticles after multiple intraperitoneal injections into rats by digital camera. Solid aggregates were found in injected body regions (a, b, c) and mesentery (d). Average-sized dots of graphene oxide nanoparticle aggregates were also localized in abdominal lipid tissue (e). Black arrows indicate graphene oxide nanoparticle aggregates. The macroscopic structure of the kidney (f), lungs (g), heart (h), spleen (i), and liver (j) were also examined. There were no macroscopic pathological features on the organs
Ex vivo digital camera images of 0.9 % NaCl solution biodistribution after multiple intraperitoneal injections into rats in the placebo group. There were no pathological changes in injected body regions (a, b) or in the mesentery (c). The macroscopic structures of the kidney (d), lungs (e), heart (f), spleen (g), and liver (h) showed no toxic impact of physiological saline solution injection
Accumulation of nanoparticles was noticeable in the body tissues of all CNP-treated groups (Figs. 4a–e, 5a–e, i, 6a–e, 8, and 9). The largest solid aggregates (up to 10 mm in diameter) were in the proximity of the injection site in the stomach serous membrane, between the connective tissues of the abdominal skin, muscles, and peritoneum (Figs. 4a–c, 5a–c, 6a–c, and 8). Numerous smaller, spherical-shaped aggregates (diameters around 2 mm) were lodged among the mesentery, to a lesser extent in DN (Fig. 4d) than in the GN (Fig. 5d) and GO (Fig. 6d) groups, where the mesenteries were almost black due to their burden of nanoparticles. Smaller aggregates were observed in abdominal lipid tissue in the proximity of the injection site and mesentery (Figs. 4e, 5i, 6e, and 8). Moreover, in connective and lipid tissue in the proximity of the spleen serosa, small aggregates of GN (Fig. 5i) and GO (Fig. 9a, 9b) were observed. Most of them were small dots (<1 μm in diameter) formed in groups (around 2 mm in diameter), which could be the beginning of a process forming larger aggregates. In the proximity of connective and lipid tissue in the liver serosa, small aggregates (up to 1 mm in diameter) and dots (up to 1 μm in diameter) were observed in the GN group (Fig. 9c, d). No CNP aggregates were found in the kidneys, suggesting that CNP aggregates were unable to penetrate to retroperitoneal organs through adventitia. In the control group, there were no pathological changes surrounding the injection region (Fig. 7a, b) or among the mesentery (Fig. 7c). Moreover, the control group mesentery was much better supplied with blood and had larger blood vessels than in the CNP groups.
Visualization of CNP aggregates in the proximity of collected organs by stereomicroscopy. In the connective and lipid tissue of the spleen serosa, small dots (1 μm), and groups (up to 2 mm) of graphene oxide nanoparticle aggregates were formed (a) and (b). Small dots (1 μm), groups (up to 2 mm), and aggregates (up to 1 mm) of graphite nanoparticles were formed in the connective and lipid tissue of the liver serosa (c) and (d). Black arrows indicate CNP aggregates
Biochemical Serum Parameters and Hematology
To assess the systemic toxicity of CNP, a number of biochemical parameters in serum, such as aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), blood urea nitrogen (BUN), total protein, lactate dehydrogenase, triglycerides, albumins, and creatinine were measured (Table 3). In the present study, liver function was evaluated by measuring the serum levels of AST, ALT, ALP, and creatinine. Kidney function was evaluated by analysis of the BUN and creatinine values in serum. Most of the examined biochemical parameters in blood serum did not show significant differences in comparison to the control group. However, ALP and creatinine were significantly different in the GN group compared to the control group. In all groups, the level of glucose in blood serum was significantly lower than in the control group. These results indicate that GN exposure could induce toxicological effects on the liver and kidney, but DN and GO had no effects.
To assess the biocompatibility of CNP, chosen hematological parameters were measured (Table 4). The present results were compared with reference intervals for hematological parameters in diet-restricted 8 to 16-week-old Wistar rats collected under isoflurane anesthesia for female provided by Charles River Laboratories (Senneville, Canada). Most of the hematological parameters remained within the reference range, but the number of red blood cells, hemoglobin, hematocrit, and mean cell hemoglobin concentration dipped slightly when relative distribution width of the red cell population slightly exceed up.
Discussion
In the present experiment, we chose a relatively high dose (4 mg/kg BW) and multiple intraperitoneal injections (eight times) of nanoparticles to evaluate potential harmful effects on animal growth and health status. Since CNP are very small, we expected that it would be difficult to observe their distribution in animal organs by conventional microscopy, but surprisingly, DN, GN, and GO formed agglomerates that could be seen even by the naked human eye (Figs. 4a–e, 5a–e, i, 6a–e, 8, and 9). Probably because CNP are hydrophobic and aggregate readily, it is difficult to disperse them in living organisms. We did not observe any signs of inflammation, necrosis, or tissue reaction in the vicinity of injections. None of the excised organs showed any abnormalities after CNP administration (Figs. 4f–j, 5f–j, and 6f–j). It should also be noted that feed intake and body gain were not significantly different between any of the groups.
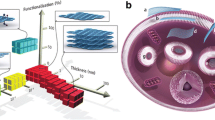
The majority of CNP aggregates were positioned around the injection region, while only small CNP dots were among the mesentery (DN, GO, GN) and in the proximity of the spleen (GN, GO) and liver (GN) serosa. There was no evidence of CNP being present in the kidney, lungs, heart, and their surroundings. It was previously reported that nanodiamond (ND) administered by intratracheal instillation were distributed mainly in the spleen, liver, bones, heart, and lungs [23] (Table 5). However, in mice intratracheally instilled with even a higher dose (20 mg/kg) than in our experiments (4 mg/kg), no ND were found in the liver and spleen [12]. This difference may be due to the different sources and production methods of ND. In another work by Yuan et al. [24], the distribution of ND after intravenous injection was studied in mice by using 125I-labeled ND. The stability of 125I-ND was greater than 90 % within 25 h, and the in vivo distribution showed that ND predominantly accumulated in the liver, spleen, and lung. About 60 % of the injected ND was found in the mouse liver at 0.5 h post injection, and this level stayed constant over 28 days [24]. Rojas et al. [13] labeled DN with another radionuclide, 18F, to study their in vivo biodistribution. The results showed that the intravenously injected DN were mainly distributed in the lung, spleen, and liver, and excreted into the urinary tract. Their research further indicated that the addition of surfactant agents did not change this distribution pattern significantly, except for a slight reduction in the urinary excretion rate of DN. It was also found that after removing DN with a larger particle size by filtration, uptake of DN was completely inhibited in the lung and spleen and significantly reduced in the liver [13]. 60Co-Co/graphitic-shell nanocrystals (60Co-Co/GC) were accumulated in mouse lung, liver, and spleen at 1, 6, 12, 18, and 24 h after intravenous injection, with the highest accumulation at 6 h but a low distribution in other tissues at all times. Moreover, 60Co-Co/GC began to eliminate slowly from lung and liver after 6 h, but there was a gradual increase in the spleen from 12 to 24 h [25]. However, it was reported that feeding of suspensions and microinjection of fluorescent ND into the gonads of C. elegans causes no harm [26]. Furthermore, there was no significant microscopic difference between the fluorescent ND-treated and control groups except for the presence of carbon-laden macrophage clusters on the peritoneal surface of the ND-treated animals [27]. Likewise, single-walled carbon nanotubes remained in the liver and spleen for over 3 months after intravenous injection [28]. Similar results and administration routes were reported for multi-walled carbon nanotubes (MWCNT). Tween 80-dispersed MWCNT accumulated in the liver and spleen with a short blood circulation time [27]. The simply dispersed MWCNT were easily recognized by macrophages and cleared from the blood very fast, and this characteristic limits their application for drug delivery [29]. In all reports of CNP biodistribution, the liver and spleen are listed as places where the nanoparticles are present but also, depending on the administration route, nanoparticles were encountered in lung, bones, and heart (Table 5). The present results also identified the liver and spleen serosa as places where nanoparticles were present, but after multiple intraperitoneal injections into rats, solid aggregates were found mainly in proximity to the injection site in the stomach serous membrane among the mesentery (Figs. 4a–c, 5a–c, 6a–c, and 8). We observed that, although CNP have good biocompatibility [30–32], they still represent a foreign non-degradable material for biological organisms. The present results and references (Table 5) indicate that the distribution of CNP in vivo involves the blood circulation for systemic translocation of CNP and for the mononuclear phagocyte system (MPS) to remove CNP from the blood. Based on the present results, we propose a scheme regarding the fate of CNP in vivo after intraperitoneal injection (Fig. 10).
Carbon nanoparticles’ fate in vivo after intraperitoneal injection. CNP aggregates were observed in the proximity of the injection site in the stomach serous membrane and localized among the mesentery. The mesentery blood circulation system governed carbon nanoparticle trafficking and systemic translocation. The superior mesenteric vein and the splenic vein come together to form the hepatic portal vein and transport CNP to the liver and spleen, which are mononuclear phagocyte system (MPS) organs. This uptake mechanism involves macrophages in snatching up CNP from blood vessels
The blood circulation is the vehicle for CNP systemic translocation and tissue distribution. Upon administration, the blood circulation is presumably the first barrier against carbon nanoparticles, which means that blood cells have primary responsibility for governing carbon nanoparticle trafficking and systemic translocation. We investigated whether CNP could pose side effects to blood cells after intraperitoneal injection. Our data confirmed previous results by Qu et al. [33] that CNP do not exert acute toxicity on blood cells, which might be partly due to rapid clearance of nanoparticles from the circulation. However, Puzyr et al. [34] reported toxic effects on blood parameters after intravenous injection of RUDDM (Real-Dzerzhinsk ultra-disperse diamond modified) to rabbit.
The mesentery blood circulation leads to the liver, where the superior mesenteric vein and the splenic vein come together to form the hepatic portal vein. The liver is the primary organ for detoxification, defending living organisms against toxic agents; hence, it is often used in tests of the toxicity of nanomaterials [35]. Because of CNPs localizing in the liver serosa, biochemical parameters of blood serum (AST, ALT, and creatinine) reflecting hepatic injury were measured. The data obtained from the hepatotoxicity biomarker study clearly showed that GN significantly increased the activity of serum ALP and creatinine compared to the control group. However, there were no abnormalities or toxic impacts of DN and GO on rat liver. The results from the literature are conflicting. Measurements of tissue morphology and biochemical parameters in mice treated intratracheally with DN indicated dose-dependent toxicity to the lung, liver, kidney, and blood [23]. In contrast, Puzyr et al.[34] found no indications of inflammatory processes 3 months after subcutaneous exposure to RUDDM in mice, but when studied in rabbits, a number of blood biochemical parameters were affected after intravenous administration of RUDDM, suggesting that the exposure route could influence the toxic effects of RUDDM.
In the connective and lipid tissue in the proximity of the liver and spleen serosa, small aggregates of GN (Figs. 5i and 9c, d) and GO (Fig. 9a, b) were observed. As macrophages are highly concentrated in the liver and spleen, it could be possible for large numbers of GN and GO nanoparticles to accumulate in the liver and spleen serosa and in the stomach serous membrane. Such an uptake mechanism involving the mononuclear phagocyte system (MPS) is consistent with the general conception of the fate of nanoparticles in vivo [25]. The MPS recognizes nanomaterials through the binding of serum opsonin proteins to nanomaterials [33, 36]. It has been reported that carbon nanotubes were trapped by the MPS and retained mainly in the liver of mice for a long time [35, 36]. GO accumulated in the liver, with most GO aggregates localized within Kupffer cells, while no GO could be found in hepatocytes, highlighting the important role of MPS in clearing GO from the circulation [33]. CNP trapped in Kupffer cells could be excreted via bile, but the process is very slow [28].
It is thought that nanoparticles should have final hydrodynamic diameters ≤5.5 nm in order to be excreted from the rat body through the kidneys [37, 38]. In the present work, no CNP were found in the kidneys, suggesting that CNP aggregates and agglomerates were unable to penetrate the glomerular basement membrane. This might be attributed to the inability of larger particles, such as the examined nanoparticles, to cross the basement membrane. It has been demonstrated that PEGylated GO could speed up renal excretion of small marked nanoparticles [39]. Furthermore, there were no CNP aggregates in the kidneys, implying that GO could be rapidly eliminated through kidney filtration [33]. It is highly probably that single nanoparticles of DN and GN (3–4 nm) could be extracted by kidney, but larger CNP are not excreted in urine; instead, they are eliminated from the blood by the MPS and thus tend to accumulate in the spleen and liver [37, 40, 41]. Aggregation of nanoparticles could influence their ability to interact with or enter cells and thus adds complexity to the system [37]. In the present work, we did not observe the occurrence of DN, GN, or GO aggregation in the kidneys; probably, the agglomerates were not able to penetrate to retroperitoneal organs through adventitia.
Conclusions
The tested nanoparticles had no toxic effects on general animal health status, growth, overall appearance of the animal interior, organ weight, and biochemical and hematological parameters. The CNP accumulated as small dots (<1 μm in diameter) and massive agglomerates (up to 10 mm in diameter) in proximity to the injection sites. The tendency of CNP to form agglomerates is unique and could be useful in drug delivery systems to immobilize CNP and drug complexes in the targeted body regions and then slowly release active substance.
Abbreviations
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- BUN:
-
Blood urea nitrogen
- BW:
-
Body weight
- CNP:
-
Carbon nanoparticles
- DN:
-
Diamond nanoparticles
- GN:
-
Graphite nanoparticles
- GO:
-
Graphene oxide
- LDH:
-
Lactate dehydrogenase
- MPS:
-
Mononuclear phagocyte system
- MWCNT:
-
Multi-walled carbon nanotubes
- ND:
-
Nanodiamond particles
- TEM:
-
Transmission electron microscopy
- TG:
-
Triglycerides
- TP:
-
Total protein
References
Jastrzębska AM, Kurtycz P, Olszyna AR (2012) Recent advances in graphene family materials toxicity investigations. J Nanopart Res 14:1320
Schrand AM, Hens SAC, Shenderova OA (2009) Nanodiamond particles: properties and perspectives for bioapplications. Crit Rev Solid State Mater Sci 34:18–74
Zhu Z, Garcia-Gancedo L, Flewitt AJ, Xie H, Moussy F, Milne WI (2012) A critical review of glucose biosensors based on carbon nanomaterials: carbon nanotubes and graphene. Sensors (Basel) 12:5996–6022
Xiao J, Duan X, Yin Q, Zhang Z, Yu H, Li Y (2013) Nanodiamonds-mediated doxorubicin nuclear delivery to inhibit lung metastasis of breast cancer. Biomaterials 34:9648–9656
Krueger A, Lang D (2012) Functionality is key: recent progress in the surface modification of nanodiamond. Adv Funct Mater 22:890–906
Petráková V, Taylor A, Kratochvílová I, Fendrych F, Štursa J, Cígler P, Ledvina M, Fišerová A, Kneppo P (2012) Luminescence of nanodiamond driven by atomic functionalization: towards novel detection principles. Adv Funct Mater 22:812–819
Meinhardt T, Lang D, Dill H, Krueger A (2011) Pushing the functionality of diamond nanoparticles to new horizons: orthogonally functionalized nanodiamond using click chemistry. Adv Funct Mater 21:494–500
Huang H, Pierstorff E, Osawa E, Ho D (2007) Active nanodiamond hydrogels for chemotherapeutic delivery. Nano Lett 7:3305–3314
Chao J, Perevedentseva E, Chung P, Liu K, Cheng C (2007) Nanometer-sized diamond particle as a probe for biolabeling. Biophys J 93:2199–2208
Fu C, Lee H, Chen K, Lim T, Wu H, Lin P, Wei P, Tsao P, Chang H, Fann W (2007) Characterization and application of single fluorescent nanodiamonds as cellular biomarkers. PNAS 104:727–732
Huang H, Pierstorff E, Osawa E, Ho D (2008) Protein-mediated assembly of nanodiamond hydrogels into a biocompatible and biofunctional multilayer nanofilm. ACS Nano 2:203–212
Yuan Y, Wang X, Jia G, Liu J-H, Wang T, Gu Y, Yang S-T, Zhen S, Wang H, Liu Y (2010) Pulmonary toxicity and translocation of nanodiamonds in mice. Diam Relat Mater 19:291–299
Rojas S, Gispert JD, Martın R, Abad S, Menchon C (2011) Biodistribution of nanoparticles. In vivo studies based on 18 F radionuclide emission. ACS Nano 5:5552–5559
Liu K, Chen M, Chen P (2008) Alpha-bungarotoxin binding to target cell in a developing visual system by carboxylated nanodiamond. Nanotechnology 19:205102
Zanni E, De Bellis G, Bracciale MP, Broggi A, Santarelli ML, Sarto MS, Palleschi C, Uccelletti D (2012) Graphite nanoplatelets and Caenorhabditis elegans: insights from an in vivo model. Nano Lett 12:2740–2744
Yang K, Zhang S, Zhang G, Sun X, Lee S, Liu Z (2010) Graphene in mice: ultrahigh in vivo tumor uptake and efficient photothermal therapy. Nano Lett 10:3318–3323
Yang K, Gong H, Shi X, Wan J, Zhang Y, Liu Z (2013) In vivo biodistribution and toxicology of functionalized nano-graphene oxide in mice after oral and intraperitoneal administration. Biomaterials 34:2787–2795
Yang K, Wan J, Zhang S, Tian B, Zhang Y, Liu Z (2012) The influence of surface chemistry and size of nanoscale graphene oxide on photothermal therapy of cancer using ultra-low laser power. Biomaterials 33:2206–2214
Yan L, Wang Y, Xu X, Zeng C, Hou J, Lin M, Xu J, Sun F, Huang X, Dai L, Lu F, Liu Y (2012) Can graphene oxide cause damage to eyesight? Chem Res Toxicol 25:1265–1270
Yang K, Liangzhu F, Shi X, Liu Z (2013) Nano-graphene in biomedicine: theranostic applications. Chem Soc Rev 42:530–547
Zhang Y, Nayak TR, Hong H, Cai W (2012) Graphene: a versatile nanoplatform for biomedical applications. Nanoscale 4:3833–3842
Kurantowicz N, Sawosz E, Jaworski S, Kutwin M, Strojny B, Wierzbicki M, Szeliga J, Hotowy A, Lipińska L, Koziński R, Jagiełło J, Chwalibog A (2015) Interaction of graphene family materials with Listeria monocytogenes and Salmonella enterica. Nanoscale Res Lett 10:23
Zhang X, Yin J, Kang C, Li J, Zhu Y, Li W, Huang Q, Zhu Z (2010) Biodistribution and toxicity of nanodiamonds in mice after intratracheal instillation. Toxicol Lett 198:237–243
Yuan Y, Chen Y, Liu J-H, Wang H, Liu Y (2009) Biodistribution and fate of nanodiamonds in vivo. Diam Relat Mater 18:95–100
Zhan L, Wei Q, Yanxia G, Junzheng X, Wangsuo W (2011) Biodistribution of 60 Co–Co/graphitic-shell nanocrystals in vivo. J Nanomater 2011:10–15
Mohan N, Chen C-S, Hsieh H-H, Wu Y-C, Chang H-C (2010) In vivo imaging and toxicity assessments of fluorescent nanodiamonds in caenorhabditis elegans. Nano Lett 10:3692–3699
Deng X, Yang S, Nie H, Wang H, Liu Y (2008) A generally adoptable radiotracing method for tracking carbon nanotubes in animals. Nanotechnology 19:075101
Yang S-T, Wang X, Jia G, Gu Y, Wang T, Nie H, Ge C, Wang H, Liu Y (2008) Long-term accumulation and low toxicity of single-walled carbon nanotubes in intravenously exposed mice. Toxicol Lett 181:182–189
Yang S-T, Luo J, Zhou Q, Wang H (2012) Pharmacokinetics, metabolism and toxicity of carbon nanotubes for biomedical purposes. Theranostics 2:271–282
Zhu Y, Li J, Li W, Zhang Y, Yang X, Chen N, Sun Y, Zhao Y, Fan C, Huang Q (2012) The biocompatibility of nanodiamonds and their application in drug delivery systems. Theranostics 2:302–312
Fiorito S, Serafino A, Andreola F, Togna A, Togna G (2006) Toxicity and biocompatibility of carbon nanoparticles. J Nanosci Nanotechnol 6:1–9
Bianco A, Kostarelos K, Prato M (2011) Making carbon nanotubes biocompatible and biodegradable. Chem Commun (Camb) 47:10182–10188
Qu G, Wang X, Liu Q, Liu R, Yin N, Ma J, Chen L, He J, Liu S, Jiang G (2013) The ex vivo and in vivo biological performances of graphene oxide and the impact of surfactant on graphene oxide’s biocompatibility. J Environ Sci 25:873–881
Puzyr AP, Baron AV, Purtov KV, Bortnikov EV, Skobelev NN (2007) Nanodiamonds with novel properties : a biological study. Diam Relat Mater 16:2124–2128
Patlolla AK, Berry A, Tchounwou PB (2011) Study of hepatotoxicity and oxidative stress in male Swiss-Webster mice exposed to functionalized multi-walled carbon nanotubes. Mol Cell Biochem 358:189–199
Liu Z, Cai W, He L, Nakayama N, Chen K, Sun X, Chen X, Dai H (2007) In vivo biodistribution and highly efficient tumour targeting of carbon nanotubes in mice. Nat Nanotechnol 2:47–52
Khan HA, Abdelhalim MAK, Al-Ayed MS, Alhomida AS (2012) Effect of gold nanoparticles on glutathione and malondialdehyde levels in liver, lung and heart of rats. Saudi J Biol Sci 19:461–464
Choi HS, Liu W, Misra P, Tanaka E, Zimmer JP, Itty Ipe B, Bawendi MG, Frangioni JV (2007) Renal clearance of quantum dots. Nat Biotechnol 25:1165–1170
Yang K, Wan ЌJ, Zhang ЌS, Zhang Y, Lee S, Liu Z (2011) In vivo pharmacokinetics, long-term biodistribution, and toxicology og PEGylated graphene in mice. ACS Nano 5:516–522
De Jong WH, Hagens WI, Krystek P, Burger MC, Sips AJ, Geertsma RE (2008) Particle size-dependent organ distribution of gold nanoparticles after intravenous administration. Biomaterials 29:1912–1919
Von Maltzahn G, Park J-H, Agrawal A, Bandaru NK, Das SK, Sailor MJ, Bhatia SN (2009) Computationally guided photothermal tumor therapy using long-circulating gold nanorod antennas. Cancer Res 69:3892–3900
Acknowledgements
This report is part of Natalia Kurantowicz’s PhD thesis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing Interests
The authors declare that they have no competing interests.
Authors’ Contributions
NK designed and performed the experiments with rats, analyzed the data, and wrote the paper. BS participated in the experiments with rats, performed the TEM analyses, and wrote the paper. ES conceived the study and helped draft the manuscript. SJ participated in the administration of nanoparticles and animal euthanasia. MK participated in the statistical analysis. MG and MW participated in the experiments and TEM analyses. LL prepared and characterized the GO used in the experiments. KM prepared and characterized the DN. AC participated in the design and coordination and helped draft the manuscript. All authors read and approved the final manuscript.
Authors’ Information
NK, BS, SJ, and MK are PhD students at the Warsaw University of Life Sciences (WULS). ES is a DSc, professor, and head of a department at WULS. MW and MG are PhD and employees at WULS. LL is a PhD, head of a department at the Institute of Electronic Materials Technology. KM is PhD and employ at the Koszalin University of Technology, AC is a DSc, professor, and head of a division at the University of Copenhagen.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kurantowicz, N., Strojny, B., Sawosz, E. et al. Biodistribution of a High Dose of Diamond, Graphite, and Graphene Oxide Nanoparticles After Multiple Intraperitoneal Injections in Rats. Nanoscale Res Lett 10, 398 (2015). https://doi.org/10.1186/s11671-015-1107-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s11671-015-1107-9